 A. Blythe Ryerson, MPH, PHD, Interim Chief, Cancer Surveillance Branch, Centers for Disease Control and Prevention (NAACCR Committee Member)
A. Blythe Ryerson, MPH, PHD, Interim Chief, Cancer Surveillance Branch, Centers for Disease Control and Prevention (NAACCR Committee Member)
(770) 488-2426; [email protected]
I’m pleased to announce the release of this year’s Report to the Nation, an annual collaborative effort by CDC, NCI, ACS, and NAACCR. This 18th “edition” has CDC as the lead agency; however, its success relies upon the tremendous expertise from senior researchers across all the collaborative organizations. Furthermore, no major cancer surveillance report would be possible without the continued dedication and contributions of the state and regional cancer registry staff collecting the data for analysis.
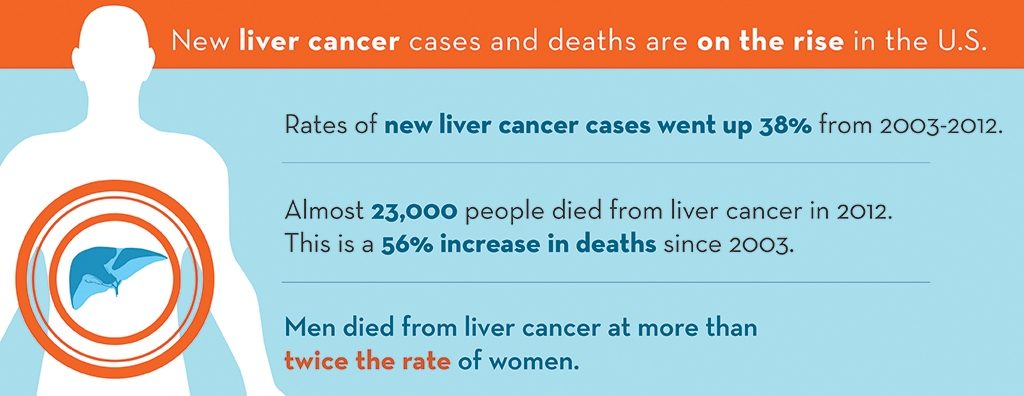
Despite successful reductions in the occurrence and mortality from the most common cancers, some cancers are showing unfavorable trends. Liver cancer, the special focus of the report, has death rates increasing at the highest rate of all cancer sites among men and women, and liver cancer incidence rates are rising at a rate second only to those of thyroid cancer.
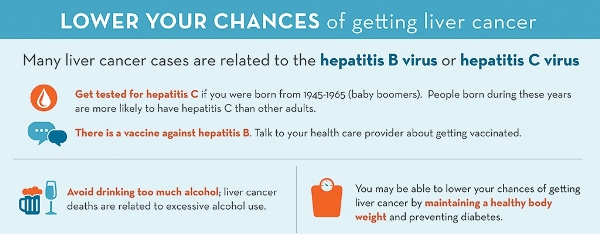
A major risk factor for liver cancer is hepatitis C virus (HCV) infection. About 22% of the most common histological type of liver cancer is attributed to HCV. Because rates of chronic HCV infection are most common among people born 1945-1965, CDC recommends one-time testing for HCV for people born during this time. Those who test positive should be referred for appropriate care and treatment. Other strategies for reducing the burden of liver cancer include promoting hepatitis B vaccination, establishing and implementing public health initiatives aimed at reducing unhealthy behaviors such as smoking and excessive alcohol use, and promoting health eating and physical activity to reduce obesity.
Moderate media interest in the topic helped bring attention to the report, including from U.S. News and World Report and multiple national and statewide media outlets. You can read the whole report here. Take a look at the graphics (free for reposting) at www.cdc.gov/cancer.
Abstract
Background: Annual updates on cancer occurrence and trends in the United States are provided through an ongoing collaboration among the American Cancer Society (ACS), the Centers for Disease Control and Prevention (CDC), the National Cancer Institute (NCI), and the North American Association of Central Cancer Registries (NAACCR). This annual report highlights the increasing burden of liver and intrahepatic bile duct (liver) cancers.
Methods: Cancer incidence data were obtained from the CDC, NCI, and NAACCR; data about cancer deaths were obtained from the CDC’s National Center for Health Statistics (NCHS). Annual percent changes in incidence and death rates (age-adjusted to the 2000 US Standard Population) for all cancers combined and for the leading cancers among men and women were estimated by joinpoint analysis of long-term trends (incidence for 1992-2012 and mortality for 1975-2012) and short-term trends (2008-2012). In-depth analysis of liver cancer incidence included an age-period-cohort analysis and an incidence-based estimation of person-years of life lost because of the disease. By using NCHS multiple causes of death data, hepatitis C virus (HCV) and liver cancer-associated death rates were examined from 1999 through 2013.
Results: Among men and women of all major racial and ethnic groups, death rates continued to decline for all cancers combined and for most cancer sites; the overall cancer death rate (for both sexes combined) decreased by 1.5% per year from 2003 to 2012. Overall, incidence rates decreased among men and remained stable among women from 2003 to 2012. Among both men and women, deaths from liver cancer increased at the highest rate of all cancer sites, and liver cancer incidence rates increased sharply, second only to thyroid cancer. Men had more than twice the incidence rate of liver cancer than women, and rates increased with age for both sexes. Among non-Hispanic (NH) white, NH black, and Hispanic men and women, liver cancer incidence rates were higher for persons born after the 1938 to 1947 birth cohort. In contrast, there was a minimal birth cohort effect for NH Asian and Pacific Islanders (APIs). NH black men and Hispanic men had the lowest median age at death (60 and 62 years, respectively) and the highest average person-years of life lost per death (21 and 20 years, respectively) from liver cancer. HCV and liver cancer-associated death rates were highest among decedents who were born during 1945 through 1965.
Conclusions: Overall, cancer incidence and mortality declined among men; and, although cancer incidence was stable among women, mortality declined. The burden of liver cancer is growing and is not equally distributed throughout the population. Efforts to vaccinate populations that are vulnerable to hepatitis B virus (HBV) infection and to identify and treat those living with HCV or HBV infection, metabolic conditions, alcoholic liver disease, or other causes of cirrhosis can be effective in reducing the incidence and mortality of liver cancer. Cancer 2016. ©2016 American Cancer Society.
The opinions expressed in this article are those of the authors and may not represent the official positions of NAACCR.
